The pancreas is a gland behind your stomach and in front of your spine. It produces enzymes that help break down food and hormones that control blood sugar levels.
Pancreatic cancer usually begins in these cells. It forms when cells grow out of control and create a tumor. Tumors may be malignant (cancerous) or benign (not cancerous).
Two kinds of pancreatic cancer
About 95% of pancreatic cancers begin in the cells that produce digestive enzymes. This is known as exocrine pancreatic cancer.
Only about 5% of pancreatic cancers begin in the cells that produce hormones. These are known as endocrine pancreatic cancer. Tumors that form in these cells are called pancreatic neuroendocrine tumors (NETs). Pancreatic NETs have a better prognosis (outcome or course of a disease).
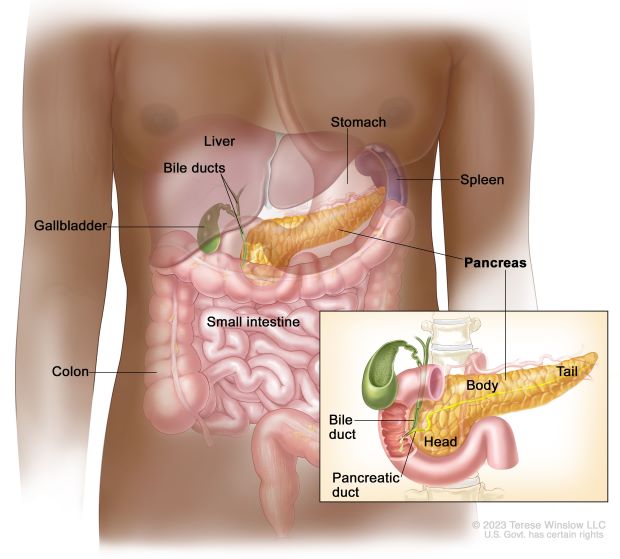
Source: National Cancer Institute
Who is at risk?
There are many risk factors for pancreatic cancer, including:
- Smoking
- Having excess body weight
- Having a personal history of diabetes or chronic pancreatitis (inflamed pancreas)
- Having a family history of pancreatic cancer or pancreatitis
- Having certain hereditary conditions, such as Lynch syndrome or hereditary breast and ovarian cancer syndrome
What are the signs and symptoms?
Pancreatic cancer is hard to spot early because it may not cause any signs or symptoms. As the cancer grows, possible symptoms include:
- Jaundice (yellowing of the skin and whites of the eyes)
- Light-colored stools
- Dark urine
- Pain in the upper or middle abdomen and back
- Weight loss for no known reason
- Loss of appetite
- Fatigue
Pancreatic NETs may have different signs and symptoms. They may also cause the body to make too much of the hormone cortisol, leading to Cushing syndrome.
These symptoms may be caused by other conditions, too, so it’s important to discuss any concerns with your doctor.
How is it diagnosed?
Your doctor will likely do a physical exam and ask you about your symptoms and family health history.
Diagnosis is usually done with imaging and other tests to see the pancreas and the area around it. Examples of these tests include ultrasounds, MRIs, CT scans, and taking samples of blood, urine, and tissue. This helps a doctor determine whether it is cancer and, if so, the cancer’s stage (how the tumor has grown or spread).
Many people get a second opinion to help with diagnosis and talk about treatment options. The National Cancer Institute’s (NCI) Cancer Information Service can help you find a doctor or hospital or with getting a second opinion.

A doctor can diagnose pancreatic cancer with imaging and other tests. Many patients will get a second opinion to confirm a diagnosis and discuss treatment options.
How is it treated?
Treating pancreatic cancer is determined by the cancer’s stage and may include surgery, chemotherapy, radiation therapy, chemoradiation therapy, or targeted therapy. You and your care team can also plan for how to manage side effects from the treatments and any cancer-related pain.
Researchers around the world are studying new ways to identify pancreatic cancer earlier and improve treatments with support from NCI. Their work includes clinical trials to test these methods and palliative care techniques to improve patients’ quality of life.
Getting support
If you or a loved one are diagnosed with pancreatic cancer, there are many resources available that can help. NCI has advice for managing treatment and its side effects, finding emotional support, and managing daily life. Learn more about coping with cancer on the institute’s website.