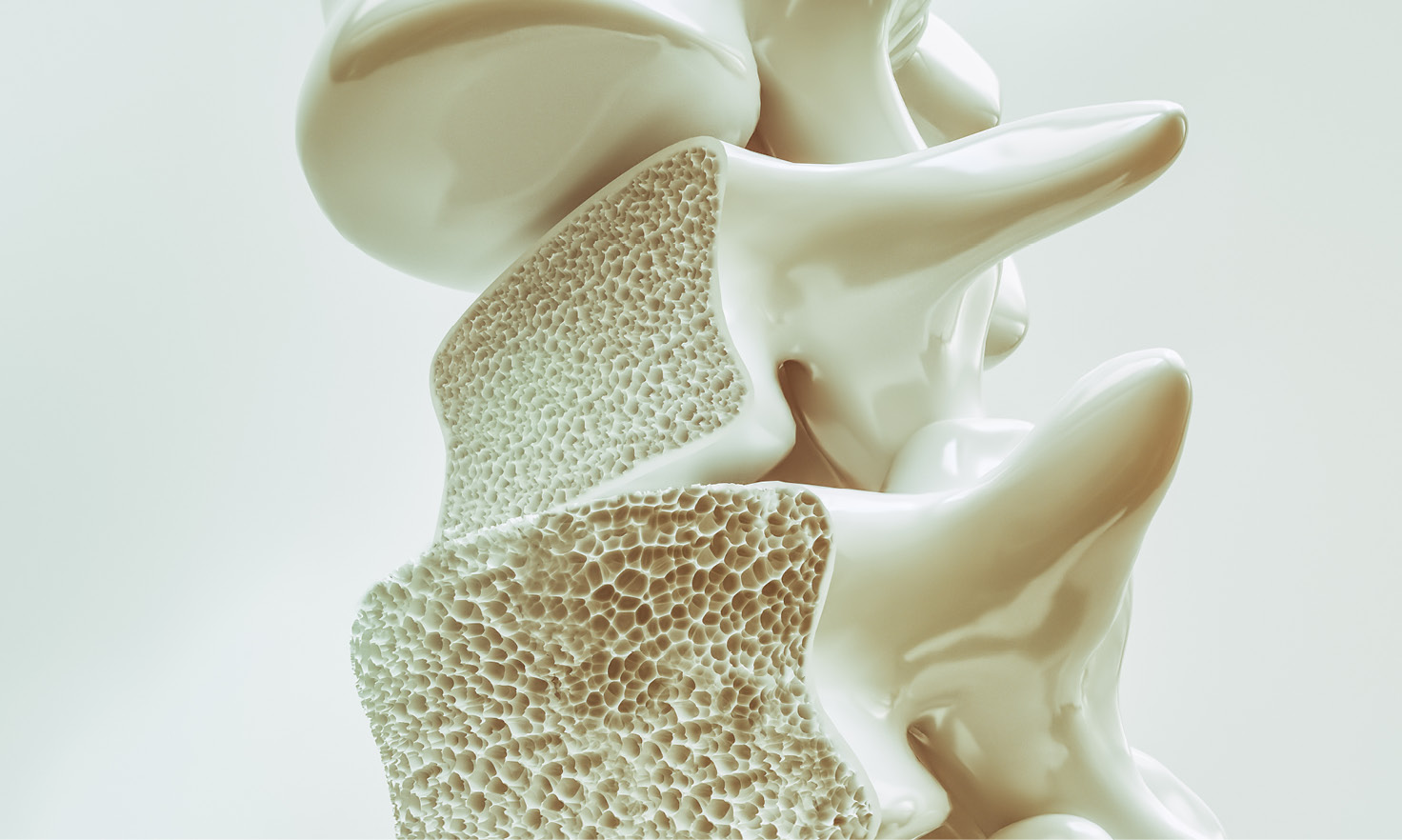
Did you know that our bones are living tissue? To keep them strong, our bodies break down old bone and replace them with new bone. When we are young, we build more bone than we break down. But as we get older, bone can break down more often than it gets replaced. This can lead to osteoporosis.
Osteoporosis can develop if your bone mass decreases or the structure of your bones changes. Osteoporosis makes your bones weak and more likely to fracture (break).
Osteoporosis is called a “silent” disease because it doesn’t show any obvious symptoms. Many people do not know they have it until they break a bone after a minor injury or movement. Something as simple as falling from standing height, bending, lifting, or even intense coughing may cause a fracture. Osteoporosis can develop in any bone, but it's most common in the bones of your hips, wrists, and vertebrae in the spine.
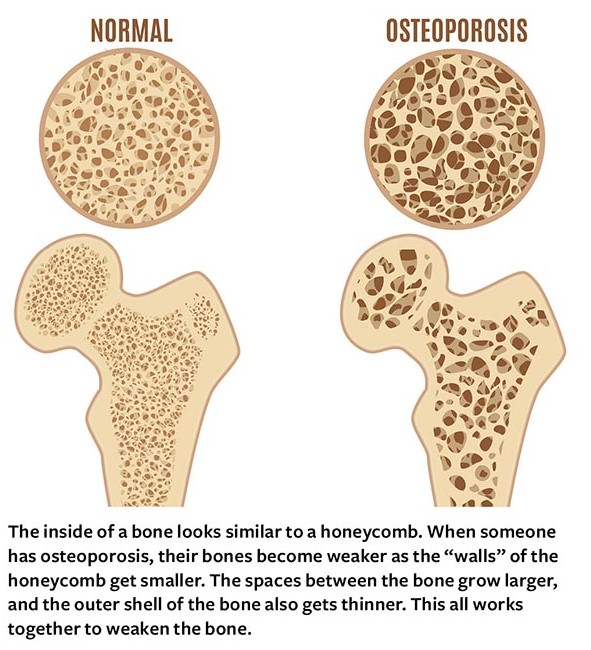
For larger image, click here.
Who is at risk for osteoporosis?
While anyone can develop osteoporosis, the risk increases as you get older. Osteoporosis is more common in people with any of these risk factors:
- Sex. Women are more likely to have osteoporosis than men, especially after menopause. White and Asian women are at the highest risk. African American and Hispanic women are at a slightly lower risk. While men are less likely to have osteoporosis, White men are at a higher risk than other groups of their sex.
- Age. As you age, you lose more bone than you build. Women over age 65 are recommended to get screened for osteoporosis by their health provider. There are no official screening recommendations for men, but their risk increases after age 70.*
- Family history. Having a parent with osteoporosis or hip fracture increases risk.
- Body type. Being slim or thin-boned increases risk because there is less bone to lose.
- Hormones. Hormone levels can affect risk for both men and women. Low estrogen levels in women due to menopause, hormone disorders, or extreme physical activity can weaken bones. Low levels of testosterone in men also raises their risk for osteoporosis.
- Nutrition. A diet low in calcium, vitamin D, or protein can raise risk.
- Lifestyle factors. These include heavy alcohol use, smoking, not being physically active, or being on bedrest for extended periods of time can all raise risk.
- Medications. Long-term use of some medications may increase risk. These include corticosteroids, proton pump inhibitors, and medicines to treat epilepsy. Some cancer medications and glucocorticoid steroids can also increase risk.
- Medical conditions. Some medical conditions increase risk, including:
- Endocrine diseases
- Certain digestive diseases, such as IBS
- Rheumatoid arthritis
- Certain types of cancer
- HIV
- Anorexia nervosa
How is osteoporosis diagnosed?
A health care provider can usually diagnose osteoporosis with a routine screening. They may ask you about your medical and family history and whether you have ever broken a bone. They may also want to know if you have lost height or weight or if you are losing muscle strength. Talk to your doctor if your posture, balance, and gait (how you walk) have changed.
The most common test for osteoporosis is a bone mineral density test, which measures how strong your bones are and predicts your risk of bone fractures.
How is osteoporosis treated?
If you have the disease, your doctor will likely recommend treatment designed to slow or stop bone loss and help prevent fractures. They may recommend eating a balanced diet with enough calcium, vitamin D, and protein. They may also recommend other lifestyle changes or prescribe medicine to slow bone loss or rebuild bone. Medications can cause side effects, so talk to your doctor or pharmacist if you have questions about what you’re taking.
Regular physical activity is important if you have osteoporosis, but certain activities may put a strain on high-risk parts of the body. Avoid high-impact exercise and movements that twist your spine (like swinging a golf club) or heavily bend the waist (like sit-ups and toe touches). A physical therapist, rehabilitation medicine specialist, or physiologist can help you make a safe exercise program. Caregivers can also help someone with osteoporosis exercise in a safe way.
Can it be prevented?
Keeping bones strong throughout your life can help lower your risk for osteoporosis, so eat a healthy diet rich in calcium and vitamin D, get regular physical activity, limit alcohol intake, and don’t smoke. It’s also important to have regular checkups and tell your doctor if you’ve had a fall or broken a bone.
Living with osteoporosis
Whether you have osteoporosis or are trying to prevent it, proper nutrition and certain exercises are good for bone health. Strong muscles help you balance and reduce your risk of falling or breaking bones. People tend to lose muscle as they age, but a combination of weight-bearing exercises, resistance training, and balance training can help. Talk to your health care provider about what’s best for you before starting any exercise program.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases also has information on exercising for bone health.
If you have osteoporosis, talk with others who have it and reach out to family and friends for support. Learning about the disease can equip you to participate in decisions about your care and help preserve your mobility and independence!
*Editor’s note: As of this publication, the U.S. Preventive Services Task Force’s osteoporosis screening recommendations are under review. Learn more about the review process and updates here.