First, thank yourself for getting a mammogram!
Breast cancer is the second most common type of cancer in women in the United States, and a mammogram, which is an x-ray of the breast, is one of the best ways to detect it. Getting mammograms at recommended times, even if you don’t have symptoms, is key to finding breast cancer early.
Detecting it early means more effective treatment options and better outcomes. Women between ages 50 and 69 who get mammograms have a lower chance of dying from breast cancer than women who do not get them.
Second, get follow-up tests as recommended by your doctor
“Abnormal” is how doctors describe a mammogram that shows something has changed in your breast. To find out what’s causing the changes, your provider may recommend diagnostic tests. These would be additional imaging tests such as an ultrasound or a magnetic resonance imaging (MRI) scan.
Your doctor may order a breast biopsy as well. A biopsy is a procedure where a small sample of cells, fluids, or tissue is taken and examined under a microscope. The test happens in a doctor’s office, clinic, or hospital (but you can go home the same day).
Third, don’t panic
Fewer than 10% of women called back for more tests after a mammogram are found to have breast cancer. But if your mammogram is abnormal, it’s important to determine what’s going on inside your body.
There are several reasons for changes in a breast, including lumps, nipple discharge, and its skin (such as itching, redness, or dimples). These variations can happen throughout your life for reasons other than cancer:
- Before or during your period (if you have one), your breasts may feel painful, swollen, or tender. You may feel lumps before your period because of extra fluid in your breasts.
- During pregnancy, you may feel breast lumps because the glands that produce milk are increasing in number and getting larger.
- As you approach menopause (during the time called perimenopause), your hormone levels change, which can make your breasts feel tender or lumpy.
- If you are taking hormones (such as hormone replacement therapy, birth control pills, or injections), your breasts may become denser. This can make a mammogram harder to interpret.
- After menopause, your hormone levels drop and you may stop having lumps, pain, or nipple discharge.
Even if you’re not due for a mammogram, talk to your doctor about breast changes as they occur.
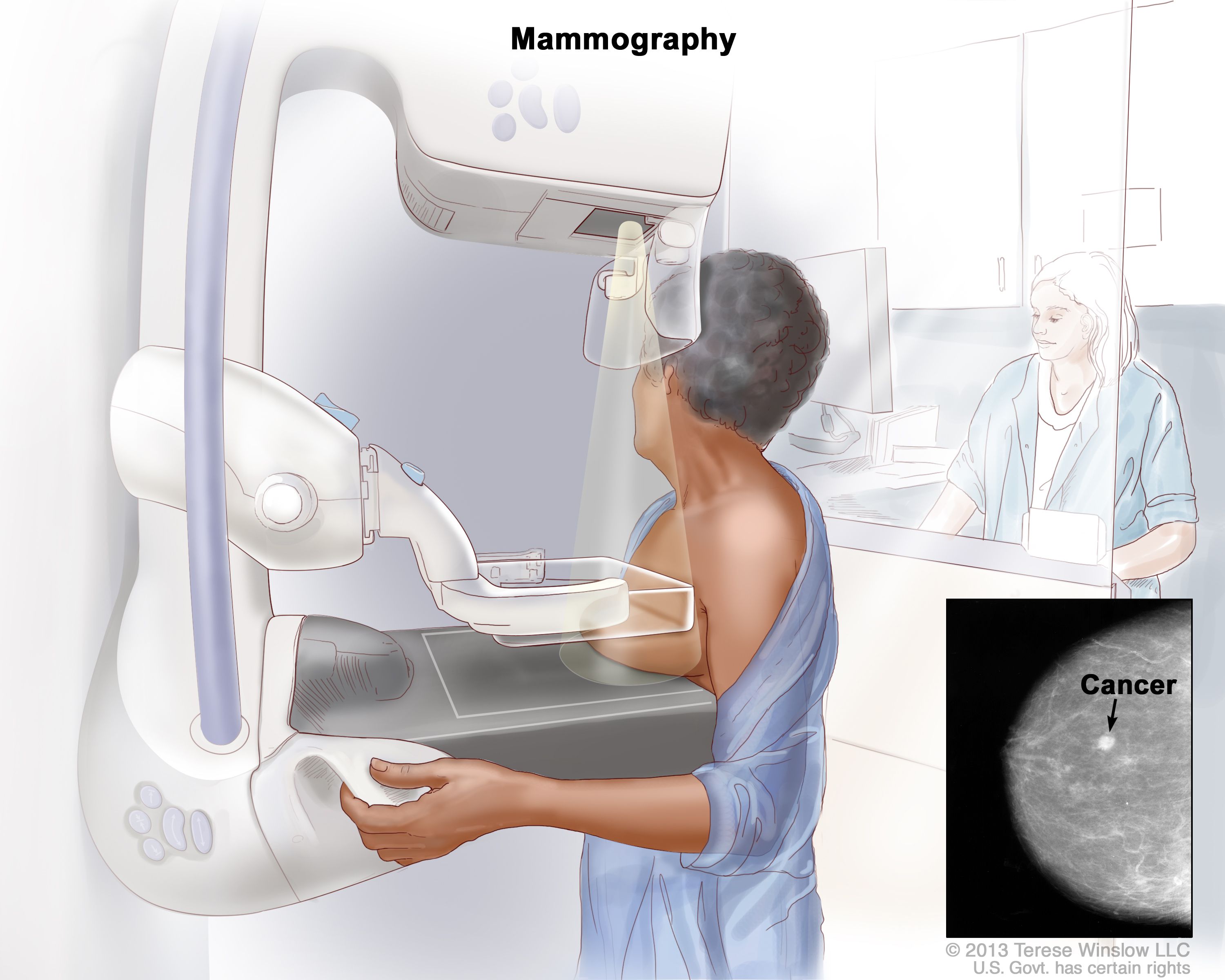
During a mammogram, the breast is pressed between two plates. X-rays are used to take pictures of breast tissue.
How mammograms work
A mammogram is a breast cancer screening test that takes an x-ray of the breasts. During a mammogram, a patient undresses from the waist up and places one breast at a time on a flat surface that has an x-ray plate. Then a machine called a compressor presses against the breast to make it flatter. The machine does this again from different angles so that the radiologist can see the inside of the breast more clearly. This can feel uncomfortable if the compressor feels cold or presses the breast firmly.
Fourth, know that other things can show up on a mammogram
There are several benign (noncancerous) breast conditions that may be visible on a mammogram. Here are a few:
- Adenosis. This is a lump caused by enlarged breast lobules (glands that make breast milk).
- Cysts. These are pockets of tissue filled with fluid that may become painful before your period.
- Blocked breast ducts. If a blocked duct becomes infected, you may feel a lump under the nipple.
- Hematoma. This is when blood clots under the skin. It may cause a lump, fever, and breast inflammation.
- Lipoma. This is a benign tumor made of fat cells and is usually a painless, soft lump.
There are also some benign breast conditions that are not cancer but may increase your risk for cancer:
- Complex fibroadenomas. This is a benign tumor that usually forms in the breast and is made up of fibrous and glandular tissue.
- Multiple intraductal breast papillomas (also called intraductal papillomas). This causes wartlike growths in the breast duct.
- Radial scars (also called complex sclerosing lesions). This is benign tissue that looks like a scar when viewed under a microscope.
- Sclerosing adenosis. This condition can cause scar-like fibrous tissue to form in the breast lobules.
You can find more information about breast changes and conditions in this guide from the National Cancer Institute, available online and as a PDF download.
If you get follow-up tests after an abnormal mammogram, talk to your doctor about the results. Even if you don’t have breast cancer, your doctor may recommend you get your next mammogram at a more specific time than the general guideline, which is every other year for women ages 40 to 74. Staying on top of preventive care is important for living a longer and healthier life.
Who should get screened
In general, women ages 40 to 74 are recommended to get a mammogram every two years. But talk to your health care provider about your individual risk of breast cancer and whether a screening test is right for you. Some patients with higher risk of breast cancer may get an MRI scan in addition to a mammogram. Men can also get breast cancer, although it’s much rarer. This is more common in men between ages 60 and 70. There are no specific screening recommendations for male breast cancer but men should talk to their doctor if they notice anything unusual.







