Ever wonder why urine is yellow or why skin looks yellow in people with jaundice? Scientists have known for more than a century that urobilin is the chemical responsible for that yellow color. But the enzyme responsible for making urobilin was a mystery…until recently. Researchers at the National Library of Medicine (NLM) found the answer in an unexpected place: the gut microbiome. Their findings can help us better understand certain health conditions, how our bodies work, and why some babies get jaundice.
Why does urine look yellow?
When your body replaces old red blood cells, it creates bilirubin. This substance then moves to your gut, where it either gets absorbed back into the bloodstream or is broken down into a chemical called urobilinogen. Your kidneys then turn urobilinogen into urobilin—this makes your urine yellow.
While researchers knew about this process, one piece of the puzzle was still missing: What causes bilirubin to break down into urobilinogen? But researchers at NLM and the University of Maryland Hall Lab recently found the missing puzzle piece—a key enzyme called bilirubin reductase.
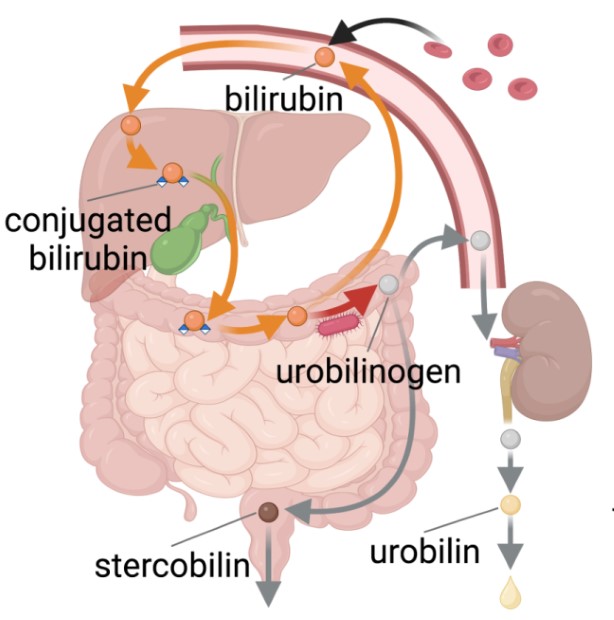
When the body breaks down red blood cells, bilirubin is produced. Bilirubin moves to the gut, where it’s either absorbed into the blood again or turned into urobilinogen. This urobilinogen is sent to the kidneys and converted to the waste product urobilin, which makes urine yellow.
How did researchers discover this?
Their first step was to find a group of bacteria that could reduce bilirubin. Many gut bacteria need low-oxygen environments to survive. This is hard to do in a lab setting, so the scientists also used computer experiments to look at the genomes of multiple bacteria at a time. A genome is the entire set of DNA instructions found in a cell. is the entire set of DNA instructions found in a cell.
Then from the bacterial genomes, researchers waded through all that bacterial data to find the gene that encoded the enzyme that breaks down bilirubin.
"We were able to confirm their functions and then look at bigger picture trends, like the relationship of that gene to different kinds of diseases," said Keith Dufault-Thompson, Ph.D., a staff scientist in NLM's Division of Intramural Research (DIR).
Why does this research matter?
Most of the time, our bodies break down bilirubin every day without any issues. But when something goes wrong, bilirubin can build up in the blood. This can lead to health problems such as jaundice, in which your skin and the whites of your eyes turn yellow. Jaundice is common in infants and people with liver disease. It can lead to pain, fevers, hearing loss, and even brain damage in severe cases.
Researchers wanted to see how the bilirubin reductase enzyme affects our health. After their discovery, they analyzed data from past studies on the gut microbiome (the ecosystem of bacteria and other microbes that live in the intestines). They took genetic samples from the microbiomes of healthy adults, young infants, and patients with inflammatory bowel disease (IBD) and searched for the gene that produces bilirubin reductase. Xiaofang Jiang, Ph.D., a principal investigator in the NLM DIR, and her team found that about 70% of infants don’t have the bacterial gene key to producing bilirubin reductase in their first month of life. This may explain why jaundice affects many newborns—their gut microbiomes aren’t as developed. The study also showed that more than 30% of adults with IBD don’t have the bacterial gene present, either.
This new research may lead to better outcomes for infants and other people with these conditions. It can also teach us more about the gut microbiome’s role in overall human health.
What’s next for this research?
Since the bilirubin reductase discovery, the research team went back to look at previous data on gut microbiomes. They want to see how the enzyme evolved in the gut environment.
Dr. Dufault-Thompson said this work could help us understand bilirubin-reducing bacteria and pave the way for new treatments. Thanks to this study, the team can learn more about what kind of functions gut bacteria can do and how they affect our bodies. These include how microbes metabolize (break down) artificial sweeteners and different types of hormones.
“These projects have helped us broaden our understanding of the impact of microbes on human health and demonstrate the wide range of functions that our microbiomes carry out,” he said.
*This article was adapted from the NLM Director’s Musings from the Mezzanine blog. Read the original article to learn more about this study and the researchers behind it.







